How 3D Bioprinting Complements the Healthcare and Pharmaceutical Industries
by Tzu-Wei (Vicki) Tsao, PhD | December 13, 2019
With recent technological advances, 3D printing has gained increasing acceptance in industries as varied as architecture, automotive and aerospace. Broadly defined as the process by which one uses a 3D model to generate a physical object, 3D printing has recently garnered more attention due to its growing utility. It has even helped the University of Maine secure three Guinness World Records for their 25-foot, 5,000-pound 3D-printed boat named 3Dirigo. Beyond enabling such eye-catching feats, 3D printing has many practical applications in the medical field specifically where it has been used to generate patient-specific dental implants and prosthetic limbs since 2012.
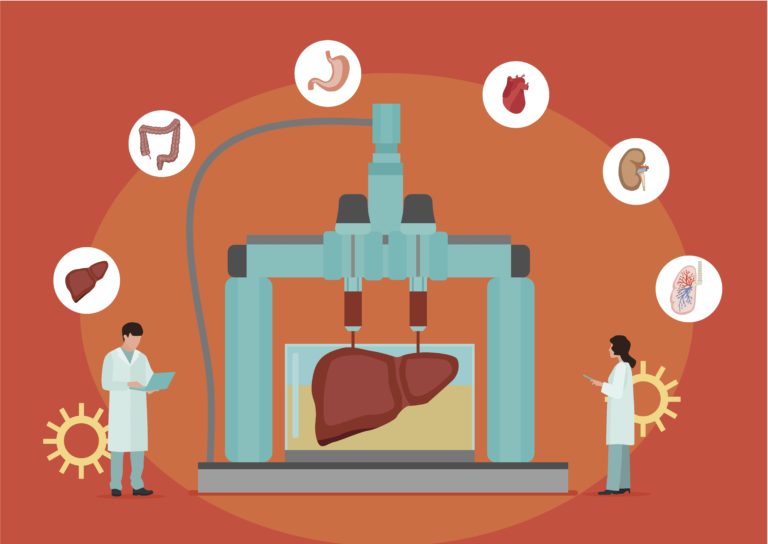
Over the past two decades, 3D printing has advanced to 3D bioprinting, a novel engineering tool that can build 3D cell constructs such as tissues or organs. 3D bioprinting is an extension of 3D printing that uses “bio-ink,” a mixture of cells and other biomaterials to construct biological materials such as functional hearts or liver tissues. There are three steps in 3D bioprinting: (1) Pre-bioprinting, the process of creating multiple layers of 2D models according to computed tomography (CT) or magnetic resonance imaging (MRI) scans, (2) Bioprinting, the actual printing process where bio-ink is used to generate cell-based pre-tissues according to the person’s medical scans, and (3) Post-bioprinting, the act of culturing and stabilizing the structure printed from the biological material by mechanical and biochemical stimulation.
Cell lines and primary cell cultures are commonly used in laboratories to elucidate biological mechanisms, test drugs, and uncover disease states. Despite the convenience of working within these platforms, these 2D monolayers of cells cannot fully represent a human body because they do not faithfully recapitulate the environment surrounding cells. These systems, for example, often neglect the important role the extracellular matrix plays in providing structural support to cells in tissues. Dr. Gail Risbridger stated in an issue of Molecular Endocrinology that “the time has come for us to culture our cells better and move from 2D to 3D models and attempt to more closely replicate the environment in which cells normally reside and then change the environment to mimic disease.” The ability of the printed constructs to more closely resemble natural tissues has spurred their application in three main areas. First, 3D bioprinting could reshape the pharmaceutical industry by dramatically lowering research and development costs by complementing pre-clinical animal models. Second, when the 3D bioprinting technique is sufficiently mature, it has the potential to solve the crisis of the current organ transplant waiting list. Third, bioprinted organs may also be deployed in medical centers to provide students- and physicians-customized training materials.
How can 3D bioprinting accelerate drug development?
Drug discovery and development is a time consuming and expensive business. The current success rate of a drug entering clinical trials is roughly 10%. Taking into consideration such low success rates, the Tufts Center for the Study of Drug Development estimated that the cost per drug from initial development to marketing is approximately $2.6 billion. Most drug candidates fail in clinical trials due to unexpected toxicity or an insufficient understanding of their underlying mechanisms in humans. Current drug discovery and disease modeling templates notably include animal models and cell lines, which cannot fully represent the human physiological and pathological environments. Even with promising results in pre-clinical studies, many drugs consequently fail in their following clinical trials.
Companies and laboratories have developed unique platforms to overcome this gap. Human induced pluripotent stem cell (iPSC)-derived neurons or human stem cell-derived organoids, for example, can mimic a more healthy tissue- or diseased tissue-based human environment and leverage pre-clinical studies to model diseases and evaluate drugs. 3D bioprinting of human tissues may also serve as a potential model that better represents human physiology to provide more accurate results. Dr. Shaochen Chen, Professor of Nanoengineering and Bioengineering Departments at the University of California, San Diego, stated that 3D bioprinted tissues are promising for drug discovery as they provide precise human tissue models that could revolutionize the fields of drug screening and disease modeling. Dr. Chen further explained that the biomaterial, including the bio-ink and the supporting gel, used for 3D bioprinting is critical and should be developed for each cell type specifically to obtain better products.
To overcome these challenges in current research fields, several biotech companies have devoted themselves to pioneering bioprinted human tissues to study different kinds of diseases. For example, the medical laboratory and research company Organovo is dedicated to designing 3D bioprinted human tissues for medical research and therapeutic applications. Their ExVive 3D-bioprinted human liver tissues have been used for in vitro studies as well as toxicology and drug testing in liver diseases. They modeled nonalcoholic fatty liver disease and TGFβ-induced fibrosis and demonstrated disease-related phenotypes on their ExVive human liver tissue platform in 2017. Allegro 3D, a 3D printing and bioprinting company located in San Diego, manufactures bioprinted human liver tissues using human iPSC-derived cells that provide personalized medicine for patient-specific disease modeling. This company also sells various bio-inks for bioprinting heart, liver, spinal cord, nerves, kidney, skin, vascular, muscle, eye, and pancreas tissues.
3D bioprinting in combination with high-throughput drug screening tests may be an ideal cell-based assay for more efficient drug discovery. Dr. Chen stated: “We need to find a better in vitro model or a functional human model that is as good as or better than current animal models. The need for 3D bioprinting is definitely in the field.” Evidently, 3D bioprinting can create a new avenue for preclinical investigations that provide an additional or better model for drug discovery.
3D bioprinting may solve the crisis of organ transplant
According to the U.S. Government Information on Organ Donation and Transplantation, more than 113,000 people are on the waiting list of national organ transplant by July 2019. One more recipient is added to the waiting list every 10 minutes, and this increment outpaces the number of eligible donors and transplants. This discrepancy is partly responsible for the death of 20 patients each day who cannot access available organs for transplant. It would be a valuable solution to the organ transplant waiting crisis if 3D bioprinters were capable to print out any human organ so that patients could receive their needed organ transplant in a timely fashion.
To begin to address these issues, the Chicago biotech start-up BIOLIFE4D successfully created a mini human heart that replicates many of the features of a functional human heart in September 2019. The mini-heart is 3D bioprinted using cardiomyocytes that were differentiated from human iPSCs. These cells were kept alive in a hydrogel system mixed together with necessary nutrient factors. The bio-ink was then loaded into the 3D bioprinter that printed out layers of the heart according to an individual’s MRI scans with some help from an internal temporary structural support. This significant milestone from BIOLIFE4D is a huge success in the race to 3D bioprint viable human organs for transplant. Given that the bio-ink is derived from the patient’s own cells and the 3D bioprinted heart is constructed exactly in the same dimensions measured from the patient’s MRI scans, the new heart will fit the patient precisely, ideally prevent the risk of rejection, and hopefully obviate additional immunosuppression treatment. Although the mini-heart was primarily intended for drug cardiotoxicity screening, its success has led to a bright future for producing a full-sized human heart suitable for transplant.
3D bioprinting for medical training purposes
While 3D bioprinting has the potential to facilitate drug discovery and organ transplants, doing so admittedly will require significantly more research and investigation. Fortunately, 3D bioprinting tissues and organs to facilitate medical training is more feasible under current regulations and business models. When a 3D-printed product is combined with different bio-materials, it can be a tool to simulate medical situations for physicians and medical students for didactic purposes. Companies can notably print a custom model tailored for individual patients, facilitating customized treatments that can help physicians target the diseased area more precisely or increase the success rate for complicated operations. Due to the rapid growth of the personalized medicine market, such custom constructs could have a blooming adoption in the near future.
In March 2019, medical researchers and orthopedic surgeons at Kaohsiung Veterans General Hospital in Taiwan announced a collaboration with the Industrial Technology Research Institute and Alliance Global Technology Company in Taiwan to establish a diagnostic platform using 3D bioprinted medical implants. This collaboration envisions 3D-printed patient-specific implants that can be applied to facilitate oral cancer patients’ reconstructive surgeries to restore soft tissues or bones that may have been removed during surgery. After consulting with doctors and fully understanding the health condition, patients could customize their own prosthetics or implants. Dr. Wen-Shin Song, Chief Physician in the Department of Neurosurgery of Cheng Hsin General Hospital at Taiwan, noted that “3D-printed customized implants are more feasible under current regulations” and represent a good starting point for future “3D bioprinting clinical applications.”
Challenges facing 3D bioprinting
Several challenges face the widespread use of 3D bioprinted tissues. For any medical application, safety must always come first. Strict regulations have to be fulfilled before 3D bioprinting can be applied to humans. In addition, the cost of future 3D-bioprinted organs is difficult to estimate, and it remains unclear how health insurance companies would handle such customized products. Moreover, scientists must develop more tissue-specific bio-inks. Companies must improve current 3D bioprinters to increase the resolution of detailed tissues. Printing speeds need to increase to keep the cells alive during the printing process and meet the needs of large-scale productions. Dr. Song also noted that “3D bioprinting could improve the pharmaceutical industry but might not completely replace current animal models.” It will be a long way before 3D bioprinting becomes the platform for drug discovery and development in the pharmaceutical industry.
Despite all these concerns, the future of 3D bioprinting is bright in light of larger industry trends towards more personalized medical treatments. As more patients demand customized therapeutics, 3D bioprinting is well suited to offering tailored tissues and organs that fit set of individualized needs. Due to its potential applications in several medical domains, 3D bioprinting is also uniquely suited to assist scientists and physicians at different stages during drug development and patient treatment. Hopefully more companies will enter this field to accelerate the technology further and capitalize on these trends.
Vicki Tsao, PhD is a Postdoctoral Scholar at the University of California, Berkeley and a Science Communication Fellow with Biotech Connection – Bay Area.


